Abstract
Introduction: The epidemiology of isolated distal deep-vein-thrombosis (d-DVT) in the calf among cancer patients is not well defined, particularly the incidence and effect on development of recurrent VTE (rVTE) and overall survival.
Methods: We used the California Cancer Registry (CCR), linked with the California Patient Discharge Database (PDD) and the Emergency Department Database (ED), which were linked to the CCR vital statistics file. Excluding patients with a prior diagnosis of VTE, we identified 760,344 first primary cancer patients diagnosed in 2005-2014 with one of the 13 most common, invasive cancers (breast, prostate, lung and bronchus, colorectal, lymphoma, urinary bladder, uterus, kidney, pancreas, stomach, ovary, myeloma, and brain). Patients with an incident cancer-associated thrombosis (CAT) diagnosis were identified if in the PDD or ED databases there was a specific ICD-9-CM code for: pulmonary embolism (PE, 415.11, 415.13. 415.19, 673.20, 673.21, 673.23, 673.24), proximal DVT (p-DVT, 451.11, 451.19, 451.81, 453.2, 453.41), distal DVT (d-DVT, 453.42), or unspecified leg DVT (nos-DVT, 453.40, 453.8 (principal diagnosis only)) or pregnancy related leg VTE (671.31, 671.33, 671.42, 671.44). The VTE location was assigned in a hierarchical fashion: PE (+/- DVT) then p-DVT, then d-DVT alone. Recurrent VTE was defined as a subsequent PDD admission with a specific ICD-9-CM VTE code in: 1) a principal diagnosis of VTE, 2) principal diagnosis of cancer and second position VTE code, or 3) secondary position of a hospital acquired VTE code. Incidence and outcomes associated with d-DVT were analyzed by cancer type. The 24-month cumulative incidence function (CIF) of first-time CAT adjusts for the competing risk of death. Multivariable Cox proportional hazards regression models were used to identify factors associated with rVTE, adjusting for the competing risk of death. The association of incident CAT location with overall survival was analyzed using multivariable Cox regression models, using CAT as a time-dependent covariate. Model covariates included sex, race/ethnicity, age at diagnosis, incident CAT location, neighborhood socioeconomic status, type of health insurance at cancer diagnosis or initial treatment, cancer stage, and initial cancer treatment (chemotherapy, radiation, and surgery); we report adjusted hazard ratios (HR) and 95% confidence intervals (CI).
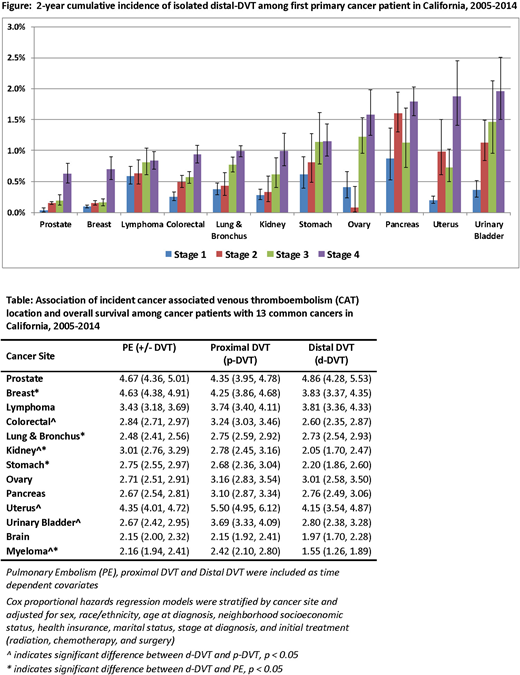
Results: Incident CAT occurred in 39,044 patients in our study (5.1%); 59.1% had PE (+/- DVT), 21.9% p-DVT, 12.1% d-DVT and 7.0% nos-DVT. Among incident CAT patients, 9.2% (n=3,587) had a rVTE, with 64.7% as PE (+/-DVT), 21.8% as p-DVT, 7.0% as d-DVT and 6.5% as nos-DVT. Among patients with incident d-DVT, 46.8% of rVTE events presented as PE, 26.1% as p-DVT and 17.8% as d-DVT. The 2-year CIF of incident d-DVT by cancer type and stage is shown in the Figure. The CIF of myeloma and brain cancers were 1.10% and 1.50%, respectively. In multivariable models assessing the impact of incident CAT location on risk of rVTE, the risk for recurrence was similar for an incident d-DVT and p-DVT for all cancers types. The risk for rVTE was similar between those with d-DVT and PE for all cancers except prostate, stomach, and ovarian, where incident d-DVT had a 50% reduced risk of rVTE compared to PE. In multivariable models considering the impact of incident CAT location on survival (Table), d-DVT was associated with worse survival among all cancer types compared to those with no CAT, with a HR that ranged from 1.55 (CI: 1.26-1.89) for myeloma to HR=4.86 (CI: 4.28-5.53) for prostate cancer. When we compared survival of incident d-DVT to p-DVT for each type of cancer, survival was similar, except for patients with colorectal [HR=0.80 (CI: 0.71-0.90)], bladder [HR=0.76, (CI: 0.63-0.91)], uterus [HR=0.75, (CI: 0.63-0.91)], kidney [HR= 0.74 (CI: 0.59-0.92)], and myeloma [HR=0.64,( CI: 0.50-0.81)] where d-DVT was associated with improved survival.
Conclusions: Isolated distal DVT cases made up only a small percentage of all diagnosed incident CAT events for all cancer types analyzed, with the 2-year cumulative incidence ranging from 0.5% - 2.0% for stage 4 patients. Subsequent rVTE events in these patients were principally PE or p-DVT (73%). D-DVT was not a significant predictor of rVTE. A diagnosis of incident d-DVT was strongly associated with worse survival, and for most cancers, survival was similar among patients with an incident p-DVT or PE.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal